
Table of Contents
Introduction
A Urinary Tract Infection (UTI) is an extremely common infection, frequently marked by a sudden, intense burning feeling when urinating, and frequent urge to use the bathroom with little output. While UTIs can range from a minor nuisance to genuinely painful, the encouraging news is that they are typically very treatable, particularly when identified early.
This guide is designed to provide a comprehensive overview of UTIs, covering how to recognize the symptoms, understand the common causes, learn about diagnosis and effective treatments, and discover practical steps for home care and prevention.
Understanding Urinary Tract Infections (UTIs)
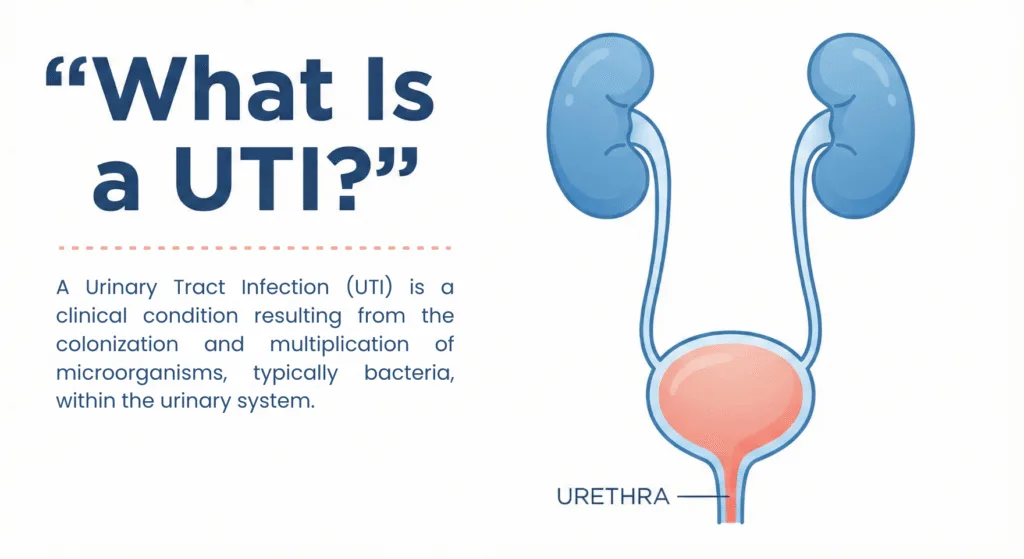
A Urinary Tract Infection (UTI) is a clinical condition resulting from the colonization and multiplication of microorganisms, typically bacteria, within the urinary system. The urinary tract functions as the body’s excretory system for the production and elimination of urine.
Anatomy of the Urinary Tract:
- Kidneys (The primary organs for urine production)
- Ureters (Ducts responsible for transporting urine from the kidneys to the bladder)
- Bladder (A reservoir for the storage of urine)
- Urethra (The terminal canal through which urine exits the body)
Most UTIs begin when bacteria travel upward through the urethra. The clinical significance of an infection’s location within the tract is crucial, as it determines both the potential severity and the appropriate management strategy.
Classification: Lower UTI vs. Upper UTI
- Lower Urinary Tract Infection (Prevalent Form)
- Primarily involves the bladder (commonly referred to as cystitis)
- Typically presents with discomfort and pain, and is generally compliant to standard treatment protocols.
- Upper Urinary Tract Infection (Clinically More Significant)
- Involves the kidneys (termed pyelonephritis)
- It is more frequently associated with systemic symptoms such as fever, flank or back pain, and carries a higher risk of complications if treatment is delayed.
Symptoms of a Urinary Tract Infection (UTI)
The onset of UTI symptoms can be subtle and subsequently intensify rapidly. While some individuals experience a predominant symptom, such as dysuria, others present with a constellation of signs.
Common UTI Symptoms
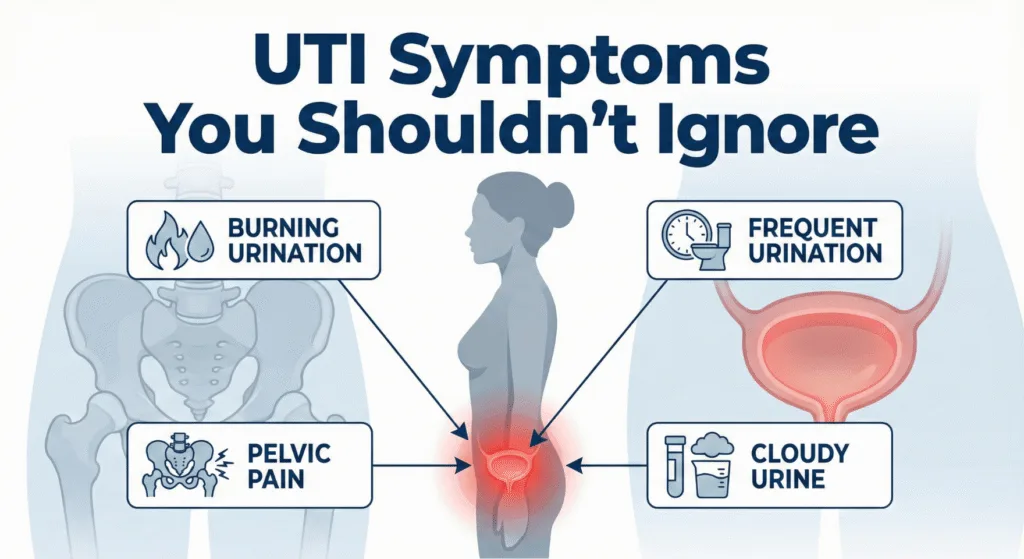
These represent the typical clinical manifestations:
- Dysuria (burning or pain during micturition)
- Urinary frequency, characterized by a persistent urge to void, often resulting in minimal output
- Urinary urgency or the sensation of incomplete bladder emptying post-micturition
- Cloudy urine or urine with a pungent, atypical odor
- Suprapubic/Pelvic discomfort (a feeling of heaviness or pressure)
Less common presentations may include:
- A generalized sense of malaise
- Mild lower abdominal discomfort without explicit dysuria
Signs Mandating Immediate Medical Attention
The presence of the following symptoms may indicate an upward progression of the infection (e.g., pyelonephritis) or increased severity:
- Fever or rigors
- Flank or costovertebral angle pain
- Nausea or vomiting
- Hematuria (blood in the urine)
- Severe weakness, confusion, or severe systemic illness
High-Risk Situations Require Early Assessment
Even in the presence of mild symptoms, a UTI should be managed with heightened vigilance in the following populations:
- Pregnant individuals
- Male patients presenting with UTI symptoms (due to lower incidence and the need for deeper etiological investigation)
- Individuals with underlying conditions such as diabetes mellitus, immunocompromise, renal disease, or a history of recurrent UTIs
- Pediatric or geriatric patients exhibiting signs suggestive of a UTI
Etiology of Urinary Tract Infections (UTIs) and Recurrence
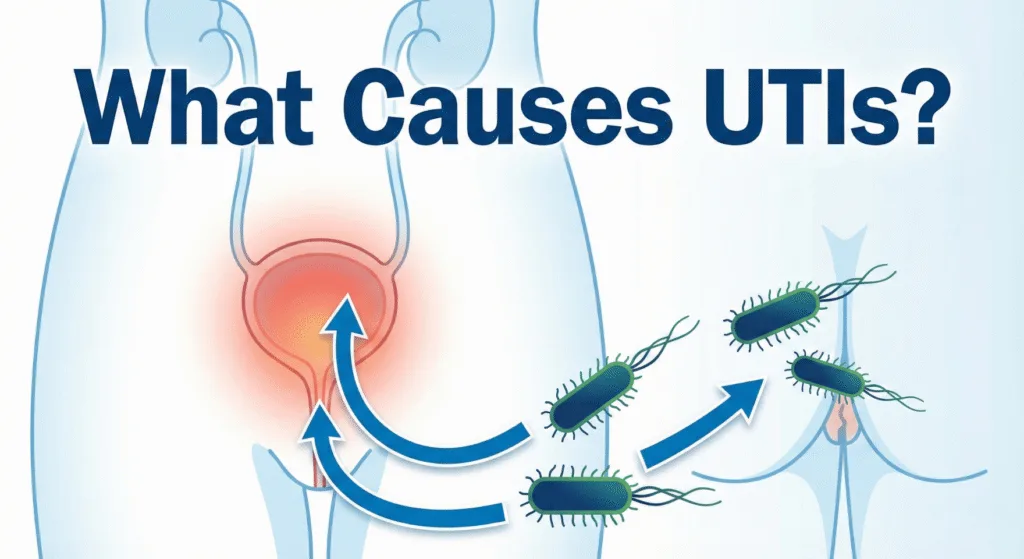
The majority of UTIs are caused by bacterial proliferation within the urinary tract. The most frequently implicated pathogen is Escherichia coli (E. coli), a bacterium commonly found in the gastrointestinal tract. This etiology is well-established and represents the most common mechanism for UTI development.
Mechanism of Bacterial Entry
Bacteria typically gain access to the urinary tract via the urethra (the conduit for urine excretion). Once established, bacterial colonization can lead to inflammation of the bladder lining, resulting in characteristic symptoms such as dysuria, urgency, and polyuria.
It is important to note that UTI development is not necessarily correlated with inadequate hygiene. Predisposing factors often include anatomical considerations, behavioral habits, and common environmental triggers.
Risk Factors: Predisposing Conditions for Urinary Tract Infections (UTIs)
- Gender (Female)
- The higher incidence in women is primarily anatomical:
- Females possess a shorter urethra, which provides a reduced distance for bacteria to ascend into the bladder.
- Sexual Intercourse
- Sexual activity can facilitate the introduction of bacteria closer to the urethral opening. This observation simply explains the temporal association between intercourse and the onset of UTIs in some individuals.
- Inadequate Fluid Intake and Urinary Retention
- Infrequent micturition (urination) allows a greater opportunity for bacterial proliferation.
- The deliberate or habitual retention of urine for extended periods can elevate the risk.
- Pregnancy
- Hormonal and physiological changes associated with pregnancy can increase susceptibility to UTIs, necessitating careful medical management during this gestation period.
- Menopause
- The decline in estrogen levels post-menopause can alter the microenvironment of the urinary tract, thereby increasing the risk of UTIs for some women.
- Obstruction or Impaired Urine Flow
- Any condition that impedes the free passage of urine elevates the risk, including:
- Nephrolithiasis (Kidney stones)
- Benign Prostatic Hyperplasia (BPH) or Enlarged prostate (in male patients)
- Any condition that impedes the free passage of urine elevates the risk, including:
- Underlying Medical Conditions (e.g., Diabetes) or Immunocompromise
- When the immune system is compromised or strained, the likelihood of developing infections, and the difficulty in their resolution, is increased.
- Use of Urinary Catheters
- The presence of a urinary catheter provides a direct route for bacterial ingress into the bladder.
- Recurrent UTIs (Repeat Infections)
- A subgroup of individuals experiences repeated infections. Common contributing factors include:
- Incomplete eradication of a preceding UTI.
- Prescribing an inappropriate antimicrobial agent for the specific pathogen.
- Failure to conduct a urine culture when clinically indicated.
- A subgroup of individuals experiences repeated infections. Common contributing factors include:
Other potential triggers include sexual activity, dehydration, changes related to menopause, or pre-existing urinary tract anomalies
Differentiating UTI from Similar Conditions (UTI vs. Yeast Infection vs. STI)
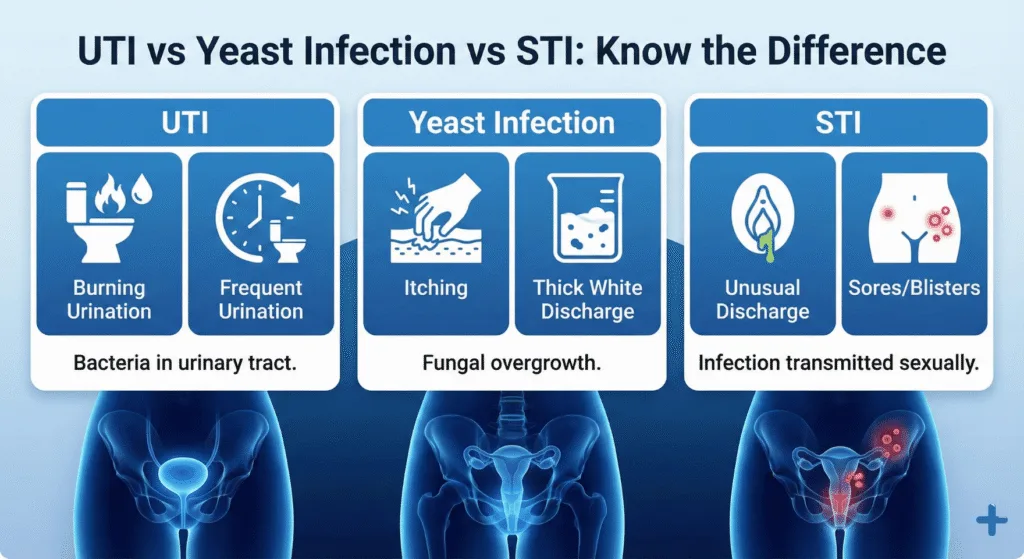
Symptomatic overlap is common, which frequently leads to diagnostic confusion. The key to differentiation lies in observing the location of the discomfort and the accompanying symptoms.
UTI vs. Candidiasis (Yeast Infection)
Symptoms Indicative of UTI Typically Include:
- Dysuria (burning sensation during urination)
- Increased urinary frequency and urgency
- Suprapubic or lower abdominal pressure
- Urine may appear cloudy or possess a strong odour
Symptoms Indicative of Candidiasis Typically Include:
- Pruritus (often intense itching)
- Burning/irritation localized to the vulvovaginal or skin area, independent of the voiding process
- Thick, white vaginal discharge (frequently described as flocculent or “cottage cheese-like”)
- Erythema or swelling around the vaginal introitus
Summary of Key Distinctions:
- The primary concern is urinary urgency combined with dysuria (UTI).
- The primary concern is pruritus combined with atypical discharge (Candidiasis).
UTI vs. Sexually Transmitted Infections (STI)
Certain STIs can manifest with dysuria, but they are generally accompanied by additional clinical indicators.
UTI signs are predominantly confined to the urinary system:
- Frequency
- Urgency
- Dysuria
- Cloudy urine
STI signs may encompass:
- Abnormal discharge (altered color or odour)
- Genital lesions, papules, or rash
- Dyspareunia (pain during sexual intercourse)
- Pelvic pain (in some cases)
- A recent change in sexual partners or a history of unprotected sexual activity (elevated risk factor)
Summary of Key Distinctions:
In the presence of atypical discharge, genital lesions, or relevant sexual risk factors, diagnostic uncertainty should be resolved through professional testing. Prompt diagnosis ensures appropriate therapeutic intervention.
Clinical Management of Uncertainty
The most pragmatic course of action is as follows:
- Obtain a urinalysis. This test is instrumental in confirming or ruling out a UTI.
- If STI exposure is a possibility, request comprehensive STI screening concurrently.
- Avoiding self-medication is crucial; treating a condition without a definitive diagnosis is ill-advised because incorrect treatment simply delays effective relief.
Diagnosis of Urinary Tract Infections (UTIs): Common Procedures
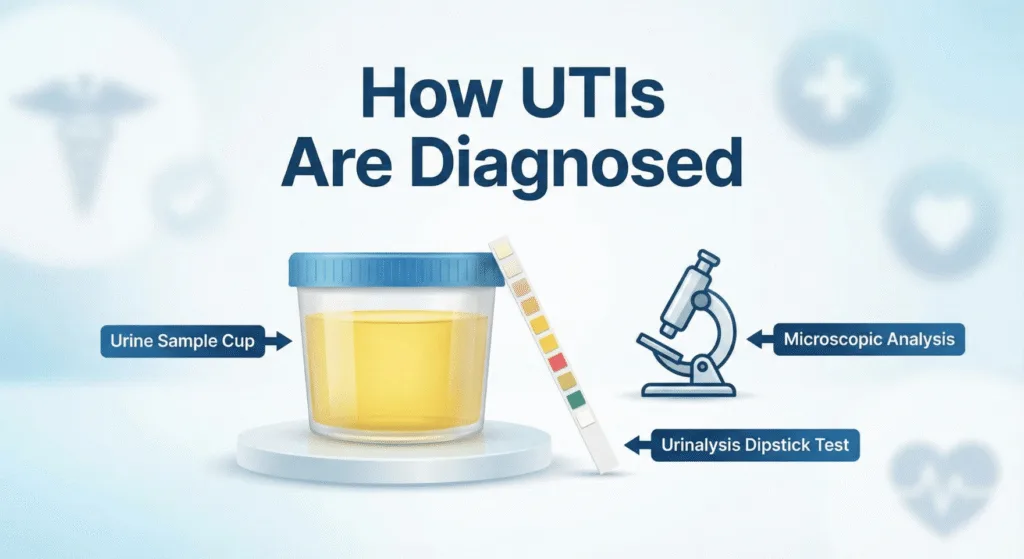
The diagnosis of a Urinary Tract Infection (UTI) is typically a straightforward process. In most instances, a physician can establish a strong preliminary diagnosis based on the patient’s presenting symptoms combined with a standard urine examination.
Urinalysis (Rapid Urine Screening): This procedure constitutes the initial and most frequent diagnostic step. A urine specimen is collected from the patient and subsequently analyzed for indicators of infection, including:
- Leukocytes (White Blood Cells): Indicative of the body’s immune response to infection.
- Nitrites: Substances often produced by the presence of certain types of bacteria.
- Hematuria (Blood): May occur as a result of inflammation or irritation.
- Other specific markers that suggest the presence of a pathological infection.
Results from the urinalysis are frequently available rapidly (sometimes during the initial consultation), which facilitates the prompt initiation of appropriate therapy.
Urine Culture (Identification and Sensitivity Testing): A urine culture requires a longer processing time (typically 1–3 days) as it involves attempting to cultivate any bacteria present in the urine sample. The principal advantages of this method are that it can identify:
- The specific bacterial organism responsible for the infection.
- The most effective antibiotics for treatment (known as antibiotic sensitivity testing).
Indications for Ordering a Urine Culture: Physicians are more likely to request a urine culture in the following circumstances:
- The patient experiences recurrent UTIs.
- Symptoms are severe or suggest the potential for a pyelonephritis (kidney infection).
- The patient is pregnant.
- The patient has underlying medical conditions that complicate UTIs (e.g., diabetes, renal disorders, immunocompromise).
- The patient’s condition failed to improve following an initial course of antibiotic treatment.
- The patient is a male presenting with UTI symptoms (often managed as potentially complicated).
Necessity of Advanced Diagnostic Imaging or Procedures: While not required for all patients, physicians may consider further evaluation if:
- UTIs continue to recur despite appropriate management.
- There are clinical signs suggestive of urinary tract obstruction (e.g., renal calculi, prostatic enlargement).
- Symptoms are consistent with a kidney infection or if initial findings are atypical.
- Symptoms persist despite negative findings on the urine tests (to investigate alternative aetiologies).
Management of Urinary Tract Infections (UTI): Efficacy and Recovery Timeline

The primary objective of UTI management is to achieve symptomatic relief and bacteriologic eradication of the infection.
Comprehensive Treatment Approach
Most UTIs, particularly cystitis (bladder infections), are managed through a dual strategy:
- Antimicrobial Therapy (to eliminate the causative bacteria)
- Supportive Care (to mitigate dysuria, pain, and general discomfort during the recovery phase)
A rapid resolution of symptoms is often observed, contingent upon the timely initiation of appropriate treatment.
Antimicrobial Agents (Primary Treatment Modality)
For confirmed bacterial UTIs, antibiotics constitute the cornerstone of therapy. Selection of the appropriate antimicrobial agent is guided by several factors:
- Patient’s clinical presentation and medical history
- Local antibiotic resistance surveillance data
- Results from a urine culture and sensitivity test (particularly in cases of recurrent or complicated UTIs)
Why you shouldn’t self-medicate
The use of residual or non-prescribed antibiotics is strongly discouraged due to the potential for adverse outcomes:
- The chosen antibiotic may be ineffective against the specific causative pathogen.
- Initial symptom abatement may occur, leading to premature cessation of treatment and subsequent infection relapse.
- Inappropriate use accelerates the development of antimicrobial resistance, complicating future management.
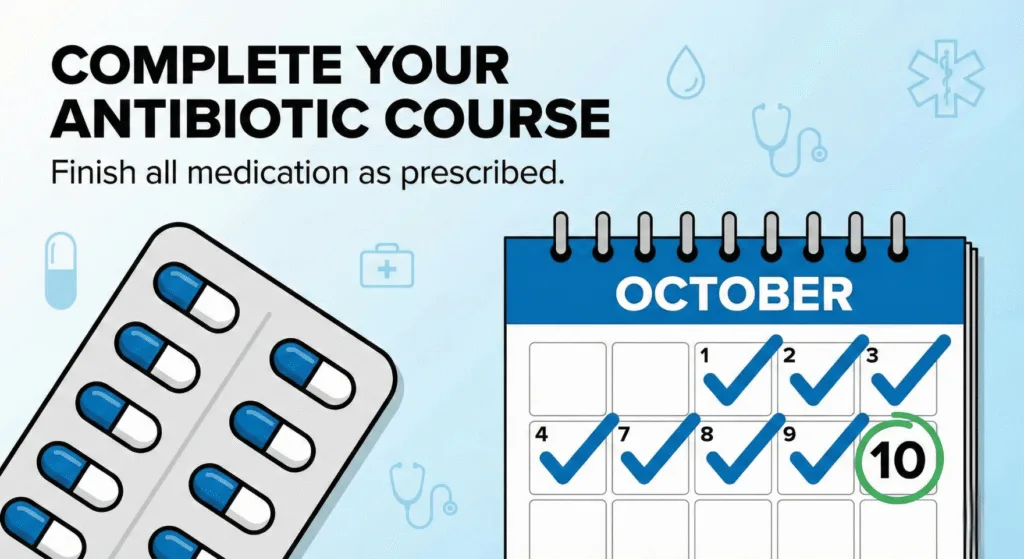
Important: finish the full course
It is imperative that the full prescribed course of antibiotics be completed, even if significant symptomatic improvement is noted within the first 24–48 hours. Premature discontinuation increases the risk of bacterial survival and infection recurrence with potentially resistant strains.
Symptomatic Relief (Supportive Measures)
While antimicrobial agents address the etiology of the infection, supportive care is essential for enhancing patient comfort and well-being.
Key supportive interventions include:
- Increased fluid intake (to promote urinary tract lavage)
- Adequate rest (to facilitate the body’s healing process)
- Prescribed analgesics for pain management (especially for pelvic or suprapubic discomfort)
- Application of localized heat (e.g., a warm compress to the lower abdomen) may provide soothing relief for some individuals.
Note: Short-term administration of urinary analgesics may be recommended by a healthcare provider to alleviate dysuria (burning upon urination). However, these agents do not possess curative properties for the infection and must be used in conjunction with a full course of antibiotics when indicated.
Expected Timeline for Symptom Resolution
For an uncomplicated bladder infection, the typical clinical course is:
- Initial symptomatic relief is commonly reported within 24–48 hours following the commencement of the correct antibiotic therapy.
- Progressive improvement of symptoms should continue over the subsequent days.
But seriously, you should get a professional check-up if:
- Symptoms fail to demonstrate improvement within 48 hours.
- The patient develops systemic signs such as fever, flank or costovertebral angle pain, or nausea/vomiting.
- Symptoms recur shortly after completing the medication.
- The patient has underlying conditions such as pregnancy, immunocompromised status, or chronic kidney disease.
Requiring Urgent Treatments
Symptoms suggestive of pyelonephritis (kidney infection), such as the presence of fever, back pain, and significant systemic illness, necessitate:
- Expedited clinical evaluation.
- The use of more potent antimicrobial regimens.
- Possible hospitalization for observation and intravenous therapy (depending on the severity of the presentation).
At-Home Care and Natural Interventions for UTIs: Efficacy and Limitations

Disclaimer: It is imperative to note that while at-home care can provide support during recovery, it generally does not serve as a substitute for antibiotic therapy in the event of a bacterial Urinary Tract Infection (UTI). Home remedies should be viewed as providing comfort and symptomatic support, rather than functioning as the primary therapeutic measure.
Nevertheless, several evidence-based actions can be undertaken at home to alleviate symptoms and facilitate the body’s recovery process.
Effective At-Home Strategies
1) Maintain Sufficient Hydration
This is the most fundamental supportive intervention:
- Increased fluid intake promotes more frequent micturition, which may aid in the mechanical expulsion of bacteria.
- Adequate hydration also slightly dilutes urine concentration, potentially mitigating the sensation of dysuria (burning).
Recommendation: Avoid excessive fluid consumption; the objective is consistent, steady hydration throughout the day.
2) Avoid Urinary Retention
- Upon experiencing the urge to micturate, one should proceed promptly. Retaining urine provides an environment conducive to bacterial proliferation.
3) Prioritize Rest and Thermal Comfort
- UTIs are often associated with systemic fatigue and malaise. Supplemental rest is genuinely beneficial for recovery.
- Applying a warm compress or heating pad to the lower abdominal region may offer relief from associated cramping or pressure for some individuals.
4) Utilize Analgesics Judiciously
- For management of discomfort, utilize pain relief options that have been approved by a healthcare professional (especially critical for patients with underlying renal conditions or other comorbidities).
- If there is uncertainty regarding the safety of an analgesic, consultation with a clinician or pharmacist is advised over self-medication.
Cranberry Consumption: An Evidence-Based Assessment
The popularity of cranberry as a remedy is considerable, but its role requires a realistic interpretation:
- It may contribute to the reduction of recurrence in certain individuals (functioning more as a preventative measure than a curative one).
- It is not considered a reliable treatment for an active, symptomatic infection.
- If utilized, it should be regarded as an adjunct to the primary treatment plan, not the central strategy.
Note for Diabetics: Patients with diabetes should exercise caution with sugary cranberry juices; unsweetened formulations or capsules are generally preferred.
Potential Symptom Irritants (Subjective)
Sensitivity varies among individuals, but certain substances may exacerbate symptoms for some:
- Caffeine (e.g., coffee, tea, energy drinks)
- Ethanol/Alcoholic beverages
- Foods with high spiciness content
- Highly acidic beverages (e.g., some carbonated soft drinks, citrus juices)
It is not necessary to eliminate all these items outright; rather, patients should monitor which specific substances intensify their symptoms of dysuria.
Common Counterproductive Practices (Mistakes to Avoid)
The following actions commonly impede the recovery process:
- Self-administration of leftover antibiotics or medication prescribed for another individual.
- Premature cessation of the prescribed antibiotic course upon subjective improvement of symptoms.
- Disregarding serious symptoms such as fever, flank (back) pain, or vomiting.
- Reliance upon unsubstantiated “rapid cure” claims found online.
When to Seek Immediate Medical Attention
Seek professional medical attention immediately if any of these symptoms appear:
- Fever and/or rigors (chills)
- Pain in the back or flanks (suggesting potential kidney involvement)
- Nausea and/or emesis (vomiting)
- Hematuria (blood in the urine)
- Existing pregnancy, or a history of frequent, recurrent UTIs
- Lack of symptomatic improvement within a period of 24–48 hours of home care initiation.
Dietary Recommendations During a Urinary Tract Infection (UTI)
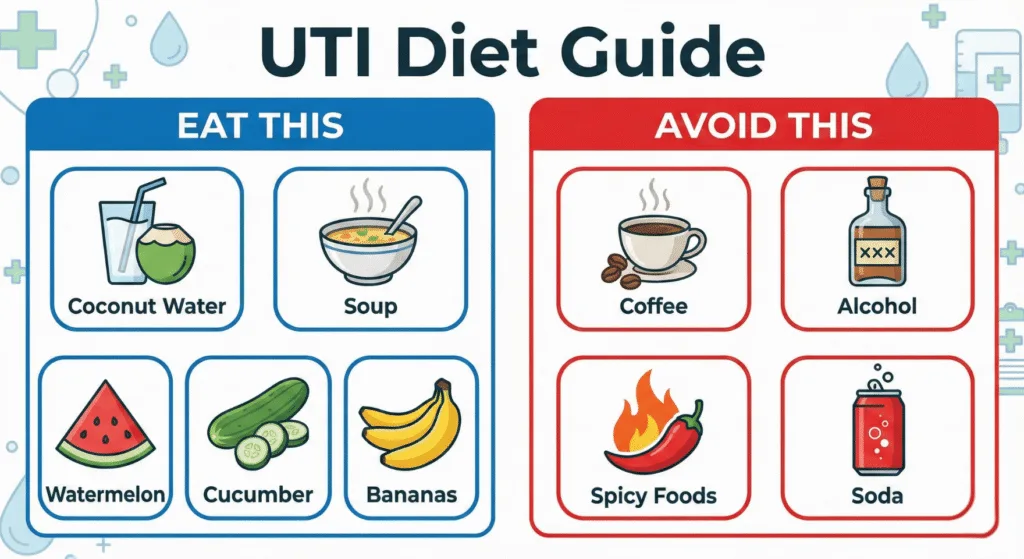
While no specific “UTI diet” offers an immediate cure, dietary intake significantly influences bladder comfort and overall well-being during recovery.
The primary focus of this guidance is: nutritional support for comfort and optimal hydration.
Recommended Focus Areas
1) Prioritize Hydration
Adequate fluid intake is the paramount concern.
- Water is essential throughout the duration of the infection.
- Alternatives to plain water include:
- coconut water (as tolerated)
- clear broths
- diluted, low-sugar electrolyte solutions
Recommendation: Consume fluids consistently in small amounts throughout the day, rather than large volumes infrequently.
2) Consumption of Bland, Soothing Foods
Heavy or complex meals may exacerbate discomfort. The following are generally well-tolerated:
- Clear soups (vegetable or chicken-based)
- Khichdi / rice and lentil combinations (easily digestible)
- Oatmeal or porridge
- Yogurt/Curd (provided dairy is well-tolerated)
- Hydrating fruits and vegetables: Bananas, watermelon, cucumber
3) Maintain Energy Levels with Protein and Simple Meals
Fatigue is a common symptom of infection; therefore, adequate caloric intake is necessary. Focus on simple, nourishing meals:
- Protein sources: eggs, lentils, lean meats, tofu, or paneer (based on dietary preference)
Foods and Beverages to Limit (If Symptoms Worsen)
These items do not cause UTIs but may intensify symptoms such as burning or urgency in susceptible individuals:
- Caffeine: coffee, strong tea, energy beverages
- Alcohol
- Highly spiced foods
- Highly acidic beverages: certain carbonated drinks, citrus-heavy juices
- Excessively sugary drinks: these can cause bladder irritation and may be contraindicated for individuals prone to infections
Complete elimination is not always necessary; however, reducing consumption of items that clearly aggravate symptoms is advised for the acute period.
Suggested Sample Meal Plan During a UTI (For Guidance)
- Morning: Warm water followed by oatmeal or porridge
- Lunch: Rice and lentil preparation (dal-chawal/khichdi) and curd
- Mid-day: A hydrating fruit snack (e.g., banana or watermelon)
- Dinner: Broth/soup paired with rice or a simple flatbread (roti) and cooked vegetable (sabzi)
- Throughout the day: Consistent intake of water, broths, or electrolyte solutions as required.
Strategies for UTI Prevention (in Cases of Recurrence)
Experiencing a single Urinary Tract Infection (UTI) establishes the primary objective: the avoidance of subsequent episodes. Prevention is achieved not through absolute perfection, but through the adoption of specific habits that mitigate the opportunities for bacteria to proliferate within the urinary tract.
1) Ensure Adequate Hydration
- Maintain regular fluid intake to ensure normal frequency of micturition (urination).
- Increased frequency of micturition reduces the duration available for bacteria to reside and multiply.
A general Guidelines: if your urine is consistently dark yellow, you may need more fluids (unless your doctor has restricted your fluids for a medical reason).
2) Avoid Prolonged Urinary Retention
Delaying urination for extended periods can elevate the risk of UTIs. Individuals who frequently defer bathroom breaks (e.g., due to professional commitments, travel, or meetings) should consider:
- Implementing a scheduled voiding routine (e.g., every 3–4 hours).
- Urinating immediately prior to lengthy travel or appointments.
3) Post-Coital Micturition (Significant for Susceptible Individuals)
For individuals prone to post-coital UTIs, this constitutes a straightforward and effective preventive measure:
- Urinate promptly following sexual intercourse to assist in flushing bacteria from the urethra.
4) Standardized Wiping and Hygiene Protocols
- Wipe the perineal area from anterior to posterior (front to back) to minimize the translocation of bacteria toward the urethra.
- Maintain gentle cleansing practices:
- Refrain from using abrasive soaps, fragranced washes, or aggressive scrubbing.
- Avoid douching, as this practice can disrupt the natural microbial balance.

5) Appropriate Clothing Choices
- Select breathable undergarments (cotton is generally recommended for comfort and airflow).
- Avoid remaining in damp or sweaty athletic attire for extended durations.
- Tight, non-breathable garments can trap moisture and potentially lead to localized irritation in some individuals.
6) Management of Recurrent UTIs: Establish a Comprehensive Plan
If UTIs are a persistent issue, consultation with a healthcare provider is warranted to investigate:
- Performance of a urine culture to identify the causative organism and determine the appropriate antibiotic regimen.
- Verification that symptoms are definitively due to a UTI each time (as irritation or sexually transmitted infections can present similarly).
- Identification of specific triggers (e.g., sexual activity, menopausal status, chronic dehydration, urinary stones, or prostate pathology in males).
- Development of a tailored prevention strategy (which may involve targeted prophylactic medication, lifestyle modifications, and guidance).
7) Specific Considerations
- Males presenting with UTI symptoms: Prompt evaluation is essential, as UTIs are less common in men and may signal underlying prostate or urinary flow abnormalities.
- Pregnancy: Immediate medical assessment is mandatory, as UTI management requires increased caution during gestation.
Frequently Asked Questions (FAQs)

The five key warning signs of a UTI are:
Burning or pain during urination
Frequent urge to urinate with little output
Cloudy or strong-smelling urine
Lower abdominal or pelvic discomfort
Blood in the urine (hematuria)
Common UTI symptoms in pregnancy include:
Burning sensation during urination
Frequent urination
Pelvic or lower abdominal pain
Cloudy or strong-smelling urine
Fever or back pain (a sign the infection may be spreading)
Pregnant individuals should seek prompt medical evaluation, even for mild symptoms.
The primary cause of a UTI is bacteria entering the urinary tract, most commonly Escherichia coli (E. coli) from the digestive system. The bacteria travel through the urethra and can multiply in the bladder.
With appropriate treatment, most uncomplicated UTIs improve within 24–48 hours, and symptoms typically resolve completely within 3–5 days.
Without treatment, symptoms may persist or worsen.
Lack of sleep does not directly cause a UTI, but poor sleep can weaken the immune system, making the body less effective at fighting infections, including UTIs.
Most bacterial UTIs require antibiotics for complete resolution.
Hydration and home remedies may ease symptoms but generally cannot fully eliminate the infection. Untreated UTIs may worsen or spread to the kidneys.
UTI symptoms often feel worse at night because:
Fluid intake decreases, making urine more concentrated
The bladder is more sensitive when lying down
Discomfort is more noticeable without daytime distractions
